May 2025
Comment la vitamine D affecte nos vies
La vitamine D est une vitamine liposoluble essentielle pour l'homme et un facteur régulateur important de l'organisme. Elle peut être stockée dans les tissus adipeux et participe à la circulation sanguine. Ses multiples effets sur l'organisme sont largement reconnus, non seulement sur le métabolisme du calcium et du phosphore, mais aussi sur les muscles, la santé cardiovasculaire, le métabolisme, l'immunité, la tumorigenèse, la grossesse, le développement fœtal, etc. Des études récentes ont montré que la vitamine D joue un rôle important dans des maladies telles que l'hypertension, les maladies cardiovasculaires, le diabète et les tumeurs.
Pourquoi la vitamine D est-elle importante ?
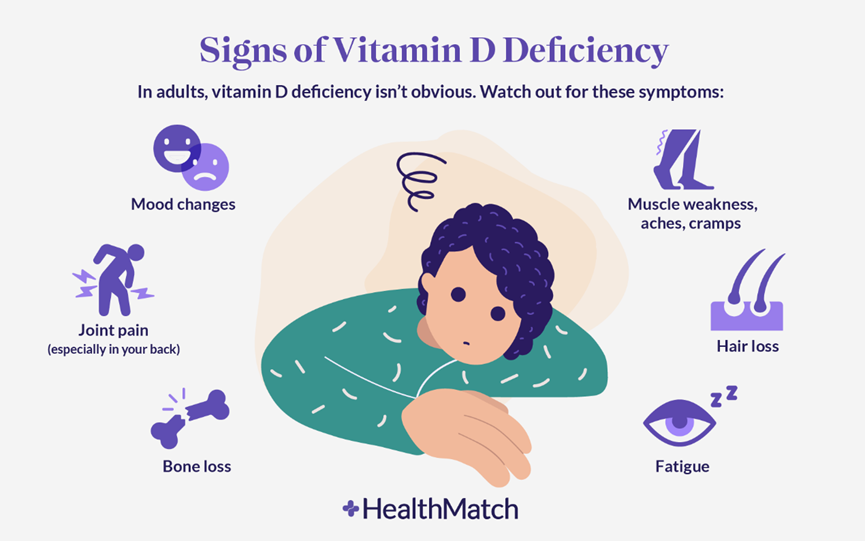
Une carence en vitamine D peut entraîner diverses maladies. Chez l'enfant, elle se manifeste principalement par le rachitisme, tandis que chez l'adulte, elle peut entraîner une ostéoporose ou une ostéomalacie, selon la gravité de la carence, et est également une cause fréquente d'hyperparathyroïdie secondaire. Chez les personnes âgées en particulier, les taux de 25-hydroxyvitamine D ont montré une corrélation significative avec une diminution de la densité minérale osseuse. Au-delà des troubles squelettiques, la recherche a identifié des associations potentielles entre la carence en vitamine D et de nombreuses autres affections, notamment certaines tumeurs malignes (comme le cancer colorectal et le cancer du sein), les maladies cardiovasculaires (hypertension, athérosclérose), les troubles métaboliques (diabète de type 2), l'insuffisance rénale chronique et les maladies auto-immunes (sclérose en plaques, polyarthrite rhumatoïde).
Comment obtenir de la vitamine D ?
Le corps humain obtient sa vitamine D par deux voies principales : l'exposition au soleil et l'alimentation. Lorsque la peau est exposée aux rayons ultraviolets B du soleil, le 7-déhydrocholestérol présent dans l'épiderme est transformé en vitamine D₃ (cholécalciférol), principale source de vitamine D pour l'homme. L'efficacité de sa synthèse dépend de facteurs tels que la situation géographique, la saison, la pigmentation de la peau et l'utilisation de crème solaire. Les sources alimentaires comprennent les aliments d'origine animale (poissons gras comme le saumon et les sardines, jaunes d'œufs, foie d'animaux et huile de foie de morue), les aliments enrichis (lait et céréales enrichis en vitamine D) et les champignons exposés aux UV (qui fournissent de la vitamine D₂). Il est à noter que la vitamine D₃ présente une biodisponibilité supérieure à celle de la vitamine D₂.

Comment notre corps produit-il de la vitamine D ?
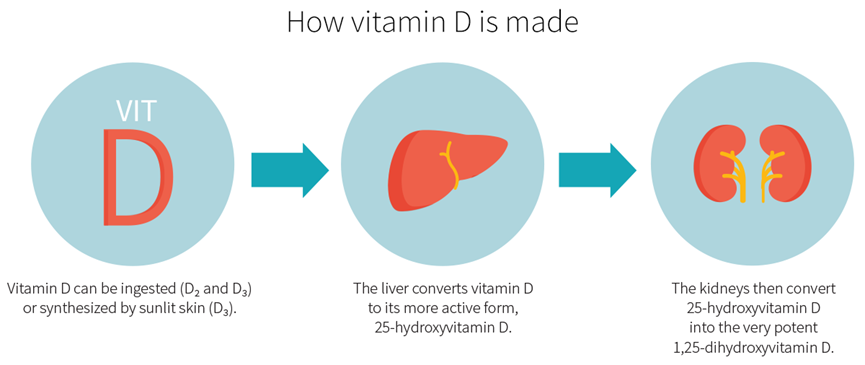
25-OH-VD La ₃ est la principale forme circulante de vitamine D dans l'organisme. Lorsque le 7-déhydrocholestérol des cellules épidermiques humaines est exposé au rayonnement solaire (UVB), il est converti en prévitamine D₃, qui s'isomérise ensuite thermiquement en vitamine D₃ (cholécalciférol). La vitamine D₃ se lie à la protéine de liaison à la vitamine D (DBP) et est transportée vers le foie, où elle est hydroxylée par le CYP2R1 (25-hydroxylase) pour former la 25-OH-VD₃. Avec une demi-vie d'environ deux semaines, la 25-OH-VD₃ constitue la référence clinique pour évaluer le statut en vitamine D. Elle est ensuite transportée vers les reins où elle est à nouveau hydroxylée par le CYP27B1 (1α-hydroxylase) pour produire la forme active, la 1,25-(OH)₂D₃ (calcitriol).
Qui devrait se faire tester ?
Personnes ayant des problèmes de santé osseuse : ostéoporose, ostéomalacie, antécédents de fractures ou enfants atteints de rachitisme.
Patients atteints de maladies chroniques : hypertension, maladies cardiovasculaires, diabète, maladies auto-immunes, maladies chroniques des reins ou du foie.
Patients atteints de cancer et groupes à haut risque : en particulier ceux atteints d’un cancer du sein, d’un cancer colorectal, d’un cancer de la prostate ou d’autres tumeurs malignes.
Personnes ayant une exposition limitée au soleil : travailleurs en intérieur, personnes alitées de longue durée, utilisateurs excessifs de crème solaire et résidents des régions de haute latitude.
Personnes obèses : la vitamine D a tendance à être séquestrée dans le tissu adipeux, ce qui entraîne une baisse des niveaux circulants.
Femmes enceintes et allaitantes : une carence peut nuire au développement du squelette du fœtus et à la santé maternelle.
Personnes âgées : déclin lié à l’âge de la synthèse cutanée de vitamine D, souvent aggravé par l’ostéoporose.
Patients sous médicaments affectant le métabolisme de la vitamine D : antiépileptiques, glucocorticoïdes, antifongiques.
Syndromes de malabsorption : Maladie inflammatoire chronique de l'intestin (maladie de Crohn, rectocolite hémorragique), maladie cœliaque, post-gastrectomie.
Test et interprétation des résultats
Le 25-OH-VD est reconnu internationalement comme l'indicateur de référence pour l'évaluation du statut nutritionnel en vitamine D. Les principales méthodes de détection actuelles comprennent l'immuno-analyse par chimioluminescence (CLIA), le dosage immuno-enzymatique (ELISA) et la chromatographie liquide couplée à la spectrométrie de masse en tandem (LC-MS/MS). Parmi ces méthodes, la CLIA est devenue la méthode la plus couramment utilisée dans les laboratoires cliniques grâce à ses avantages : forte automatisation, grande cadence de test, bonne sensibilité et forte spécificité.



ouvrez wechat et scannez le code QR. restez à l'écoute.